Why Precision-Personalised Health is Important vs. a One-Size-Fits-All Approach
Published 01/04/2024
BackWhat is Precision-Personalised Health?
Precision medicine is a patient-centric and data-driven process that is redefining healthcare delivery by specifically optimising treatment outcomes and improving patient lives. Delivering the right treatments at the right time every time to the right person is the fundamental aim of precision healthcare. This is done by focusing on an individual’s unique genetic makeup, environmental factors, and lifestyle choices in order to tailor interventions and treatment for maximum efficiency.
It’s a move away from a one-size-fits-all approach which until recently has been the best healthcare authorities could offer and makes sense given we are all unique human beings. How we respond to diets, fitness, skincare, sleep, stress management, and prescription drugs totally differs from person to person, so naturally, our approach should be unique.
Why do we accept that we all need the same amount of vitamins, minerals, and antioxidants? It’s simply due to the time and effort constraints healthcare systems are inhibited with when trying to approach personalised health. Recommended Dietary Allowances (RDAs) - you know, the figures for calories, fat, sugar, and more on all food products in the UK - are built on averages, but no one person actually falls into this category.
That low-carb diet or intermittent fasting plan might work perfectly for your friend, but that doesn’t mean it will work for you, as your bodies are different. Even identical twins with nearly identical DNA may respond to the same foods very differently. Researcher Tim Spector, a professor of genetic epidemiology at King’s College London, said: “Our recommendations, medically and public-health wise, have just been assuming that if people follow the standard plan, they’ll lose weight and develop fewer chronic diseases. Really, that thinking has now been exposed as completely flawed.”
History of Precision-Personalised Healthcare
This is not a new concept. The Greek physician Hippocrates (460-370 BC) - known as the ‘father of Western medicine’ for his contributions to medicine and founding the Hippocratic School of Medicine - supposedly advised doctors thousands of years ago to “give different ones [liquid medicines] to different patients, for the sweet ones do not benefit everyone, nor do the astringent ones, nor are all the patients able to drink the same things.” At the same time, he also suggested evaluating factors like a person’s age, physical appearance, and the time of year when prescribing medicines in order to better target drug prescriptions to individual patients.
But while Hippocrates used a person’s physique and the seasons to personalise treatments, modern science and industry hope to use your DNA. The rise of medical genetics in the latter half of the 20th century - following the discovery of the structure of DNA - has opened up the possibility of genetics providing useful insight into someone’s health and wellness responses, leading to less trial and error.
This led to the Human Genome Project - an international program whose goal was the complete mapping and understanding of all of the genes in human beings. This began in the early 1990s, and by 2003, a full sequence of around 20,500 human genes was completed and published. This historic work has had a huge impact on the way we study and treat disease, allowing us to identify the genetic basis or genomic variation of thousands of diseases whilst simultaneously dramatically improving the speed, accuracy, and accessibility of DNA and RNA sequencing.
In 2015, the concept of precision medicine was brought firmly into the public eye when US President Barack Obama exclaimed during his State of the Union address: “Tonight I am launching a new precision medicine initiative to bring us closer to curing diseases such as cancer and diabetes.” Following Obama’s comments, there was a huge increase in interest and research on precision medicine techniques, with Google reporting a x1,000 jump in searches for the term ‘precision medicine’.
In the UK, the NHS is working to become the first health service in the world to truly embrace personalised medicine. Health systems, including the US, Germany, France, Canada, Australia, and India, are also formulating policy and research programmes to support the adoption of more personalised approaches to healthcare.
Traditional Medicine vs. Precision-Personalised Medicine
Traditional medicine utilises a ‘one size fits all’ approach which means that a particular drug would be used to treat all patients suffering from a particular disease. The problem with this approach is that only a certain percentage of patients will respond positively to the particular drug, while a significant percentage will not respond positively, and another subset will actually develop negative effects. There are many reasons for the differences in reaction among people with the same disease to the same treatment, including genetic variations, age, gender, addictions, race, ethnicity, prescriptions, environmental factors, and so on.
So, unfortunately, the one-size-fits-all approach leads to a wastage of drugs, increased costs, and poor patient satisfaction. Precision medicine hopes to eradicate these issues by taking into account the genetic, environmental, and lifestyle factors among individuals in order to propose bespoke therapies.
Aiming for accurate measurement of molecular, environmental, and behavioural factors contributing to health and disease leads to more precise diagnosis, rational disease prevention strategy, treatment selection, and the development of newer therapies. Therefore, the main difference between the traditional practice of medicine and precision medicine has come about because of the availability of big data. With rapid advances in molecular biology and genetic testing becoming much quicker and cheaper, allowing researchers to collect vast swathes of data and combine them with clinical, pharmacological, and socio-economic information, analysis can be carried out using integrated data sets by various computer-based algorithms to observe patterns of effectiveness of particular treatments to specific types of people.
Precision medicine can also be tailored for population-based approaches, which lends a huge preventative angle to healthcare and seeks to engage patients as active participants in research and care, giving rise to the terminology - ‘preventive, personalised, precision, population, and participatory medicine’.
Benefits of the Personalised Healthcare Approach
The NHS has outlined how personalised healthcare has clear advantages for individual patients, populations, healthcare systems, science, and even the wider economy:
- Early Disease Detection: Disease can be detected 2-8 years before onset, and symptoms become obvious.
- Targeted Disease Prevention: The identification of predisposition markers or underlying processes to predict future disease.
- Accelerated Diagnosis: Diagnosis based on underlying cause and incidental findings - rather than just grouped symptoms.
- Targeted Therapies: Intelligent treatment pathways informed by personalised assessment of clinical effectiveness and adverse drug reactions.
They also detail the four P’s of personalised medicine:
1. Prediction and prevention of disease: By using genomic technologies and other diagnostics, those who are most at risk of disease can be identified even before the onset of their symptoms. Earlier detection opens up the prospect of new treatment options and supports people to make informed lifestyle choices, creating the potential to reduce the growing burden of disease for long-term conditions such as cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes.
2. More precise diagnoses: As it stands, a diagnosis is made based on tests and investigations into a patient’s symptoms, but although two patients may have the same symptoms, their causes could be very different. Knowledge of each individual’s complex molecular and cellular processes - informed by other clinical and diagnostic information - enables the full understanding of abnormal function and determining the true cause of symptoms. This ability to diagnose more precisely can be optimised when coupled with new and improved technologies, such as those that provide rapid and real-time results and those that can be used at the point of care. Patients and health professionals can then make shared decisions about medicines and adjust dosing in real time.
3. Targeted and personalised interventions: Personalised medicine offers the opportunity to move away from ‘trial-and-error’ care to prescribing optimal therapy first time around. Key pharmaceutical interventions are currently effective in only 30-60% of patients due to differences in how individuals respond to and metabolise medicine. Knowledge of the genetic variants responsible for individual drug response can be used to create an individual’s ‘pharmacogenomic’ profile, identifying optimal treatment.
4. More participatory role for patients: The ability for a clinician to be able to discuss information about individual genomic characteristics, lifestyle, and environmental factors and interpret personal data from wearable technology with their patients will drive a new type of conversation. They can consider lifestyle changes and when treatments might not be necessary. It may also lead patients to consider preventative measures when there is a high likelihood of a disease developing. This is a new era of medicine and requires new knowledge among professionals, patients, and the public to have confidence in using the information available to them.
Where Does Stride Fit In?
Even though health systems identify that proactive, personalised, and precision health is the future, it will be quite some time before the likes of the NHS implement this due to the sheer cost, training, and infrastructure of dealing with the UK’s estimated 67 million population as individuals that require bespoke healthcare.
Lifespan is the number of years someone lives from birth until death, while health span is the number of years someone is healthy without chronic or debilitating disease. Health systems like the NHS work hard to take care of our lifespan but when it comes to healthspan this is where Stride comes in…
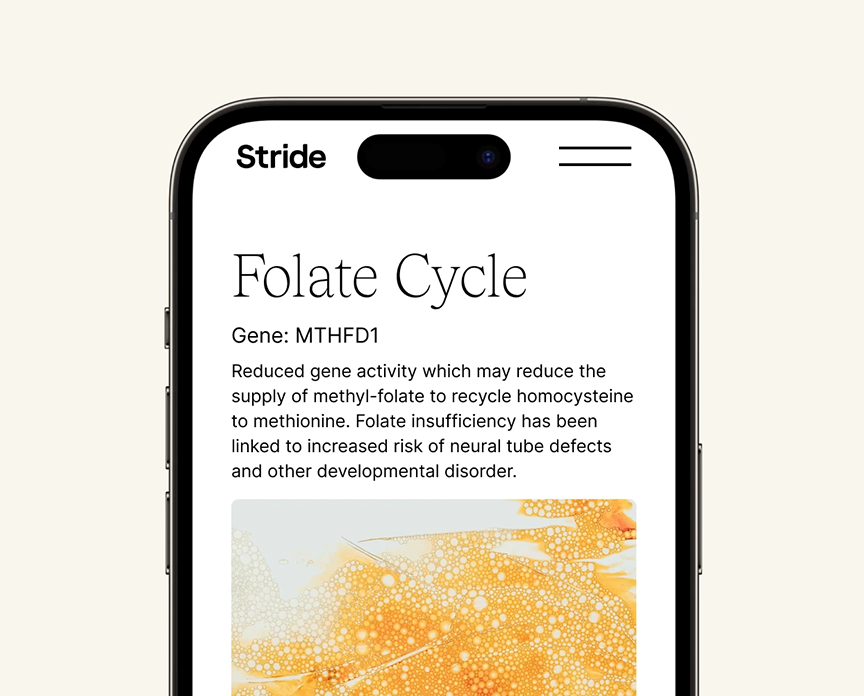
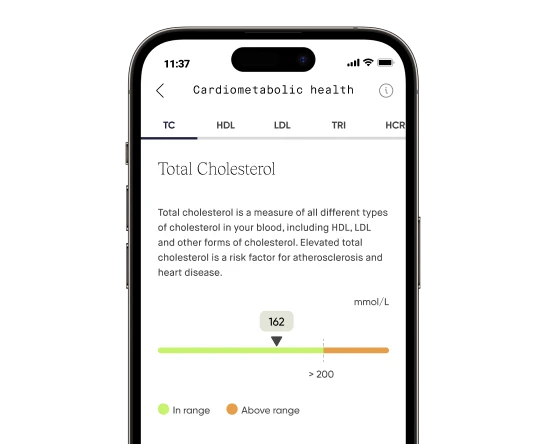
Stride is an affordable digital health ecosystem brought to you by the award-winning teams behind DNAfit and Prenetics EMEA. We offer personalised vitamin supplements, cutting-edge diagnostic testing solutions (e.g. DNA Methylation tests) from our in-house UK laboratory, expert data analysis, and comprehensive results through our advanced digital platform.
We provide our users with personalised one-to-one consultations with our dedicated dieticians to put your personalised health into practice. Our diagnostic testing reveals individual biological makeup and health needs, including genetic insights, blood biomarkers, and gut diversity (coming soon). Armed with your genetic data, we can personalise your StrideDaily vitamin supplements and provide comprehensive solutions tailored to your specific requirements - leading to proactive, effective, and sustainable health and wellness outcomes.
Benefits of StrideDaily - our personalised vitamin supplement.
Receive a cost-effective daily supplement that fills your nutrient gaps and improves your overall health with the following benefits:
- Personalised wellness, every day: StrideDaily is tailored to your unique biology, lifestyle, and goals and adapts as your needs change - keeping your health on track.
- Daily liquid shot of goodness: StrideDaily is an easy-to-drink liquid supplement—a tastier and more convenient choice than a counter full of generic, forgettable pills. It contains no artificial preservatives or caking agents.
- Pharmaceutical-grade liquid excellence: StrideDaily formulas result from a decade of rigorous research and development by our team of leading scientists and dieticians and deliver 98% nutrient absorption via our trademarked liquid liposome nutrient-delivery technology.
- At your door every month: No more spontaneous trips to anonymous health stores with bewildering choices - we bring what you need, where and when you need it.
- Choose your level of precision: From a health quiz to testing your DNA. The assessment will see you answer some questions about your general health and lifestyle, food and exercise habits, and top health goals that take just five minutes to complete.
Why unlock your genetic insights with StrideDNA?
Stride's DNA test will provide a detailed report of 150+ genetic insights, including methylation, nutrition, fitness and exercise, sleep and stress responses, and skin health genetic predispositions. An at-home saliva test kit does this, and your comprehensive and actionable genetic report will be turned around in an industry-leading 10 working days. These insights will enable you to hyper-personalise your diet plans, optimise your fitness performance, improve mental wellbeing, and understand your methylation capabilities.
Why Stride Stands Out
Stride is not just about providing personalised vitamins or DNA testing; it's about transforming your health journey. Whether you're looking for vitamins for energy, skin, immunity, or gut health, StrideDaily has you covered. Our liquid multivitamin supplements, delivered in our advanced liquid liposome format, ensure maximum absorption and efficacy. For those concerned about specific health goals, we offer supplements for recovery, digestion, and sleep. For those interested in DNA personalisation, our comprehensive genetic test unlocks your unique genetic predispositions, enabling you to tailor your lifestyle to your unique genetic needs.
Conclusion
In summary, precision-personalised health is the future of healthcare, and Stride is at the forefront of this revolution. Our personalised multivitamin approach ensures you receive the best vitamins to take daily, tailored to your unique genetic makeup and lifestyle. Join us in this journey and take strides with your health.
Get started today by visiting getstride.com.